 Meticulous attention to details in order to confirm correct patient identification and specimen identification must be performed under all circumstances. Correct patient identification is the most important step in the performance of a skin or venipuncture procedure. Common mistakes which result in improper identification include:
Meticulous attention to details in order to confirm correct patient identification and specimen identification must be performed under all circumstances. Correct patient identification is the most important step in the performance of a skin or venipuncture procedure. Common mistakes which result in improper identification include:
- Assuming that calling a patient from the waiting room by name is going to get the correct patient. Patients, who have waited a long time, who are hard of hearing, or who have English as a second language, will often hear their name at the wrong time.
- Asking patients, "Are you ____________?" Patients will smile and respond "yes" to any question that they didn't hear or don't understand.
- Moms carry all the children's medical ID cards, as well as their own. They often give the wrong child's card.
- Stopping a RN in the hallway to confirm an inpatient ID when they aren't in the patient's room and haven't seen the patient.
- A large number of specimens being double labeled. This occurs when a handwritten or stamped paper label is placed initially, and then the specimen is relabeled with a computer bar code label after order entry. Most blood banks will not accept a double labeled specimen if the original label cannot be seen.
- Trusting a person to label the specimen who did not draw the specimen. This commonly happens in the ER and on inpatient floors where the MD or RN draws the patient, but then hands it off to be labeled by other staff. Obtaining specimens from the wrong patient can lead to serious, even fatal consequences such as:
- Erroneous lab results resulting in improper diagnosis.
- Medication errors.
- Blood transfusion errors.
- Patient receives a transfusion of the wrong blood type.
- Leads to hemolytic transfusion reaction or death.
- Grounds for dismissal of the person responsible.
- Leads to malpractice lawsuit against that person and organization.
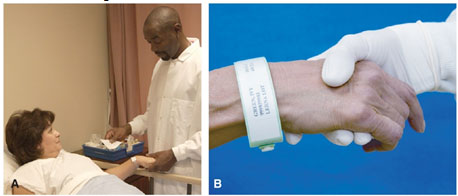
- Patient identification
- Verify name & date of birth
- Check ID bracelet
- Notify nurse of ID discrepancies
- Search for missing IDs
- Wake sleeping patients
- Ask a relative or nurse to identify a patient who is unconscious, young, mentally incompetent, or non-English speaking
Patient identification: don’t rely on nods of agreement; verify patient information with a relative or attendant


